Lower Urinary Tract Symptoms
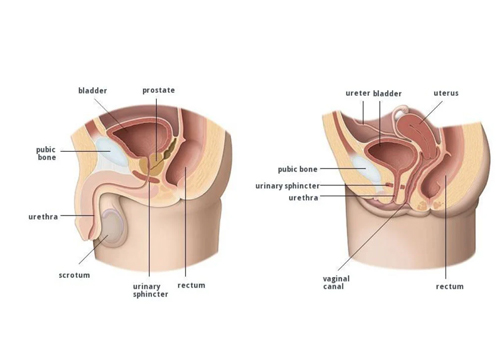
Lower Urinary Tract Symptoms (LUTS) refer to a range of symptoms related to issues with the bladder, urethra, or prostate (in men). These symptoms are broadly categorized into storage symptoms, voiding symptoms, and post-micturition symptoms. LUTS can affect both men and women, though they are often associated with benign prostatic hyperplasia (BPH) in older men.
Categories of LUTS
1. Storage Symptoms (related to bladder filling):
- Frequency: Needing to urinate more often than usual during the day.
- Nocturia: Waking up at night to urinate.
- Urgency: A sudden, strong need to urinate, sometimes with leakage (urge incontinence).
- Urinary Incontinence: Involuntary leakage of urine, including stress incontinence (e.g., leakage during coughing or laughing).
2. Voiding Symptoms (related to bladder emptying):
- Hesitancy: Difficulty starting urination.
- Weak Stream: A reduced flow of urine.
- Straining: Needing to exert effort to urinate.
- Intermittency: The stream stops and starts during urination.
3. Post-Micturition Symptoms:
- Feeling of Incomplete Emptying: A sensation that the bladder is not fully emptied.
- Post-Micturition Dribble: Leakage of urine after finishing urination.
Causes
- Benign Prostatic Hyperplasia (BPH): Enlargement of the prostate gland in men, leading to obstruction.
- Urinary Tract Infection (UTI): Infection causing irritation and inflammation.
- Bladder Overactivity: Often due to conditions like overactive bladder syndrome.
- Neurological Disorders: Diseases like Parkinson’s, multiple sclerosis, or spinal cord injuries.
- Urethral Stricture: Narrowing of the urethra.
- Pelvic Organ Prolapse: Common in women and can contribute to LUTS.
Diagnosis
- Patient History: Assessment of symptoms, their impact on quality of life, and medical history.
- Physical Examination: Includes abdominal and, in men, a digital rectal examination.
- Urinalysis: To check for infection or blood in the urine.
- Uroflowmetry: Measures the rate of urine flow.
- Bladder Diary: Tracks voiding patterns and volume.
- Imaging: Ultrasound to evaluate bladder or prostate.
- Cystoscopy: Direct visualization of the bladder and urethra if necessary.
Treatment Options
Lifestyle Modifications:
- Limiting fluid intake before bedtime.
- Reducing caffeine and alcohol.
- Weight loss if overweight.
Medications:
- Alpha-blockers: Relax the muscles in the prostate and bladder neck (e.g., tamsulosin).
- 5-Alpha-Reductase Inhibitors: Reduce prostate size (e.g., finasteride).
- Anticholinergics: Help with bladder overactivity (e.g., oxybutynin).
- Beta-3 Agonists: Improve bladder relaxation (e.g., mirabegron).
- Antibiotics: For UTIs if present.
Surgical Options:
- TURP (Transurethral Resection of the Prostate): For BPH.
- Laser Therapy: Minimally invasive option for prostate enlargement.
- Urethral Dilation or Surgery: For strictures.
- Sacral Neuromodulation: For refractory overactive bladder.
When to Seek Help
- Sudden inability to urinate (urinary retention).
- Blood in the urine.
- Significant pain or discomfort.
- Impact on quality of life or daily functioning.
If you need more detailed information about specific symptoms or treatments, feel free to ask!

