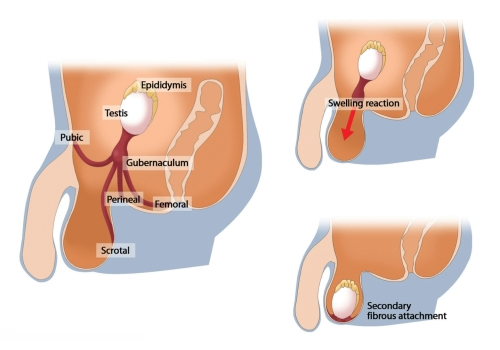
Orchidopexy is a surgical procedure used to correct cryptorchidism, a condition in which one or both testicles fail to descend into the scrotum during fetal development or shortly after birth. This procedure involves relocating the undescended testicle(s) into the scrotum and fixing it in place.
Indications for Orchidopexy
- Cryptorchidism (undescended testicle(s)), usually diagnosed in infancy or early childhood.
- Testicular torsion risk: An undescended testicle is at a higher risk of twisting and losing its blood supply.
- Infertility concerns: Testicles that remain undescended often cannot produce sperm effectively.
- Cosmetic concerns: To bring the testicle into a normal anatomical position for appearance.
Types of Orchidopexy
-
Open Orchidopexy:
- The most common form, where a surgical incision is made in the groin, and the undescended testicle is brought into the scrotum and fixed in place.
-
Laparoscopic Orchidopexy:
- A minimally invasive approach using small incisions and a camera to guide the surgery. This method is often used for intra-abdominal testicles or when the testicle is located higher up in the abdomen.
-
Microsurgical Orchidopexy:
- Involves the use of a microscope for precision surgery, especially for cases involving the blood supply to the testicle.
Procedure
- Anesthesia:
- General anesthesia is administered to the patient.
- Incision:
- For open orchidopexy, an incision is made in the groin or lower abdomen (depending on where the testicle is located).
- Testicle Mobilization:
- The undescended testicle is carefully mobilized and brought down into the scrotum.
- Fixation:
- The testicle is fixed in the scrotum using sutures to ensure it stays in place.
- Closure:
- The incision is closed, and a dressing is applied. If laparoscopic surgery is performed, the incisions are much smaller, and stitches may not be required.
Postoperative Care
- Pain Management:
- Mild to moderate pain is expected after surgery and can be managed with analgesics.
- Swelling and Bruising:
- Swelling of the scrotum and bruising may occur, but it typically resolves within 1-2 weeks.
- Activity Restrictions:
- Avoid strenuous physical activity or heavy lifting for about 2-4 weeks.
- Follow-up Visits:
- Follow-up visits are necessary to ensure proper healing and monitor for any complications such as recurrence.
Risks and Complications
- Infection: Any surgical procedure carries a risk of infection, though this is uncommon.
- Bleeding or Hematoma: Some bleeding and bruising in the scrotum can occur postoperatively.
- Recurrence: In some cases, the testicle may fail to remain in the scrotum.
- Damage to the Testicle: Rarely, the testicle may be damaged during the procedure, which can affect fertility.
- Testicular Atrophy: The testicle may shrink and become nonfunctional if the blood supply is compromised.
- Fertility Concerns: If the testicle has been undescended for a prolonged period before surgery, there may be a higher risk of reduced fertility, even after correction.
Timing of Surgery
- Early Surgery: Orchidopexy is typically recommended between 6 to 18 months of age. Early intervention helps ensure normal testicular function and reduces the risk of complications such as infertility and testicular cancer.
- Delay: If the procedure is performed later in life, especially after 2 years of age, fertility may be affected, and the testicle may not function normally, even after successful surgery.
Outcomes
- Fertility: Orchidopexy can preserve fertility in many cases, but the earlier the surgery, the better the chances of normal sperm production. If both testicles are undescended, fertility rates may be lower.
- Normal Testicle Function: Success rates for testicle survival and function are high when surgery is done early, with most children having a normal or near-normal testicle function after orchidopexy.
- Cosmetic Results: The cosmetic outcome is usually excellent, with both testicles appearing normal in size and position in the scrotum.

